February 24, 2025 report
This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
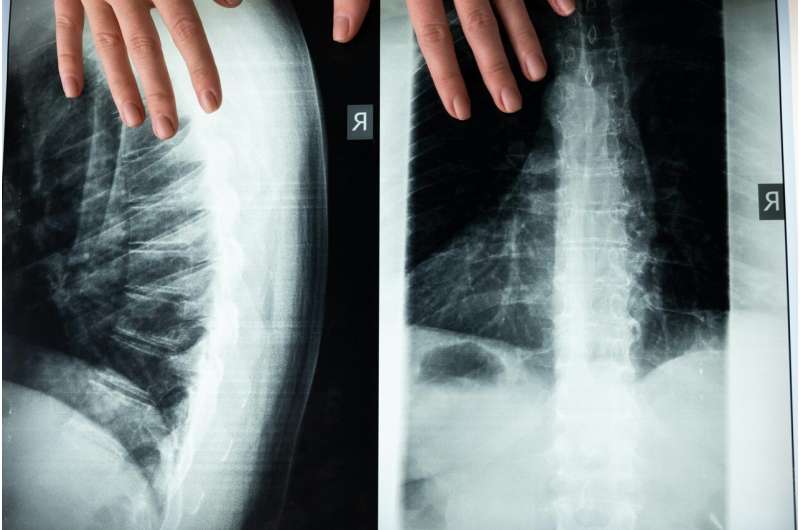
Common procedures for chronic spine pain found to offer little to no relief
Researchers from McMaster University and collaborating institutions found that commonly performed interventional procedures for chronic non-cancer spine pain may provide little to no pain relief when compared with sham procedures.
Chronic spine pain, defined as persistent pain along or referred from the spine lasting three months or longer, presents a global health challenge with significant socioeconomic implications.
While interventional procedures such as epidural steroid injections, nerve blocks, and radiofrequency nerve ablation are frequently used, clinical guidelines have offered conflicting recommendations regarding their effectiveness.
In the study, "Common interventional procedures for chronic non-cancer spine pain: a systematic review and network meta-analysis of randomized trials," published in The BMJ, researchers conducted a comprehensive search of Medline, Embase, CINAHL, CENTRAL, and Web of Science, for spine pain procedural outcome efficacy.
Eighty-one trials with 7,977 patients were included in meta-analyses out of 132 eligible studies. Patients with chronic axial or radicular spine pain were randomized to receive common interventional procedures or comparators, including sham procedures and usual care. Frequentist network meta-analyses were performed, and the GRADE approach was used to assess the certainty of evidence.
For chronic axial spine pain, moderate certainty evidence showed that epidural injection of local anesthetic, epidural injection of local anesthetic and steroids, and joint-targeted steroid injection, result in little to no difference in pain relief compared with sham procedures.
Low certainty evidence suggests minimal pain relief differences for intramuscular and joint-targeted injections of local anesthetic, with or without steroids. Intramuscular injection of local anesthetic with steroids signaled that it may actually increase pain.
For chronic radicular spine pain, moderate certainty evidence indicates that epidural injection of local anesthetic and steroids and radiofrequency of the dorsal root ganglion are unlikely to result in pain relief. Low certainty evidence suggests epidural injections of local anesthetic or steroids may also yield minimal pain relief.
In physical functioning, moderate certainty evidence shows joint-targeted injections and epidural injections with local anesthetic or steroids probably provide little to no improvement.
Low certainty evidence suggests certain procedures may slightly increase the risk of non-serious adverse events, including joint radiofrequency ablation.
When looking at the substantial cost, inconvenience, and false hope of these common procedures compared to data that suggests they are ineffective, it is unclear why they have persisted. If the study results are valid, another issue suggested is a major communication disconnect regarding procedures and patient outcomes in health care.
More information: Xiaoqin Wang et al, Common interventional procedures for chronic non-cancer spine pain: a systematic review and network meta-analysis of randomised trials, BMJ (2025). DOI: 10.1136/bmj-2024-079971
Jane C Ballantyne, Spinal interventions for chronic back pain, BMJ (2025). DOI: 10.1136/bmj.r179
© 2025 Science X Network

















